Tissue engineering involves designing scaffolds for tissue regeneration 71%
Revolutionizing Healthcare: The Power of Tissue Engineering
In recent years, tissue engineering has emerged as a promising field that holds the potential to revolutionize healthcare. This innovative approach involves designing and developing scaffolds that mimic the structure and function of natural tissues, paving the way for tissue regeneration and repair.
The Need for Tissue Regeneration
Tissue damage or loss can result from various factors such as injury, disease, or congenital defects. Traditional treatment methods often rely on transplants or prosthetics, which may not always be effective or feasible. This is where tissue engineering comes in – an innovative approach that aims to create functional tissues that can replace or repair damaged ones.
Understanding Tissue Engineering
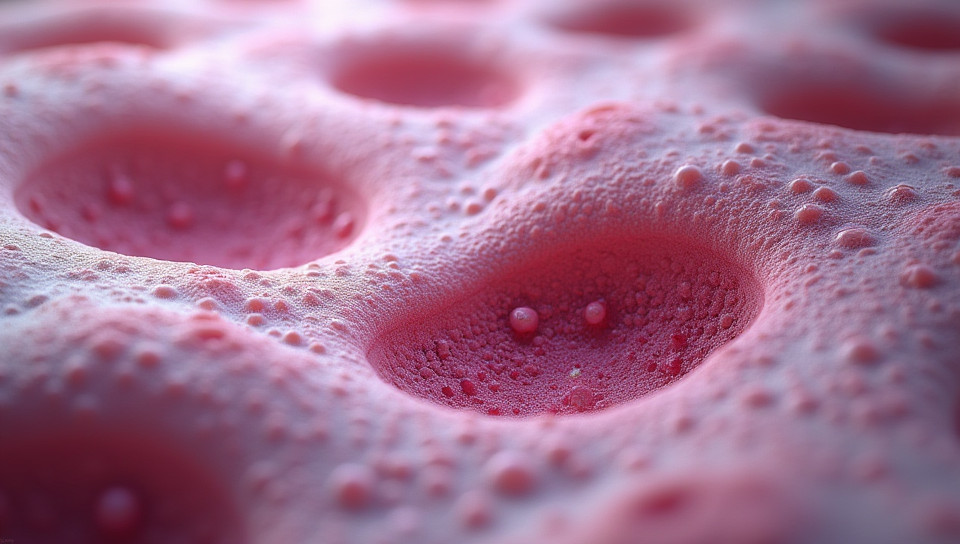
Tissue engineering involves the use of biomaterials and cells to create three-dimensional structures that support tissue growth and regeneration. These structures, known as scaffolds, serve as a template for cell attachment, proliferation, and differentiation. The scaffold must be carefully designed to mimic the natural environment of the target tissue, including its mechanical properties, biochemistry, and microarchitecture.
Key Components of Tissue Engineering
- Cell source: stem cells or progenitor cells are often used in tissue engineering due to their ability to differentiate into various cell types.
- Biomaterials: scaffolds can be made from natural or synthetic materials, such as collagen, gelatin, or polyesters.
- Growth factors: proteins that promote cell growth and differentiation are often incorporated into the scaffold design.
Challenges and Opportunities
While tissue engineering holds great promise, there are several challenges that must be addressed. These include:
- Scalability: large-scale production of scaffolds is required for widespread clinical application.
- Biocompatibility: the scaffold material must be non-toxic and biocompatible to prevent adverse reactions.
- Cellular differentiation: cells must differentiate into the correct cell type to ensure proper tissue function.
Conclusion
Tissue engineering has the potential to revolutionize healthcare by providing a novel approach to tissue regeneration. By designing scaffolds that mimic natural tissues, researchers can create functional tissues that can replace or repair damaged ones. While there are challenges to be addressed, the opportunities presented by this field make it an exciting area of research and development. As we continue to push the boundaries of what is possible with tissue engineering, we may one day see the emergence of new treatments for a wide range of medical conditions.
- Created by: Maria Thomas
- Created at: Feb. 4, 2025, 5:28 p.m.
- ID: 20090